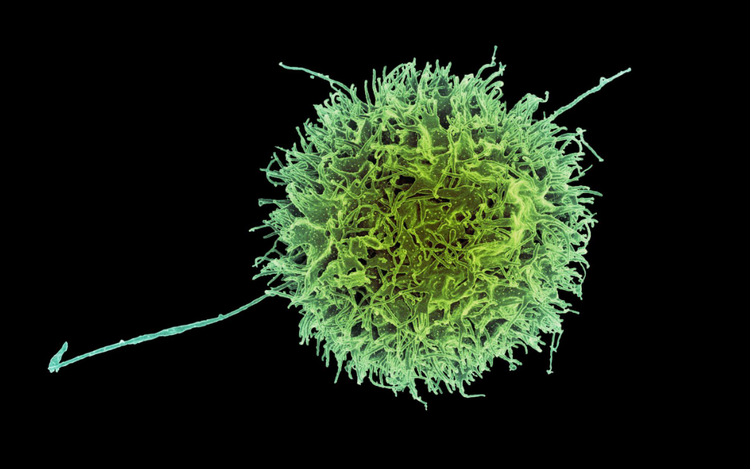
Natural killer cells help detect and destroy cancer cells as soon as they form. Photo: Supplied
Researchers at Monash University’s Biomedicine Discovery Institute, in collaboration with the Melbourne-based biotech company oNKo-Innate, have identified a gene in NK cells that, when switched off, dramatically boosts the cells' sensitivity to interleukin-15 (IL-15), a naturally occurring growth factor that plays a vital role in immune defense against cancer.
The study, published in the leading international cancer journal Cancer Cell, was led by Professor Nick Huntington and represents a significant step forward in developing more effective and less toxic immunotherapies.
IL-15 is a critical immune-signaling molecule produced by the body to stimulate the production and activity of immune cells such as NK cells.
These cells are among the first responders to abnormal cells, including emerging cancers.
However, cancer cells often evolve mechanisms to suppress immune responses, even in the presence of IL-15, allowing tumors to grow and spread unchecked.
Attempts to therapeutically enhance IL-15 signaling using drugs have led to serious side effects, as they activate immune cells throughout the body – not just in the tumor – causing widespread inflammation and toxicity.
To address this challenge, the research team used CRISPR gene-editing technology to screen for genes that, when removed, increase the sensitivity of NK cells to IL-15.
They identified a key gene that encodes an enzyme responsible for dampening the immune response.
The finding opens the door to developing safer and more targeted cancer treatments, said Professor Huntington.
The enzyme encoded by the newly identified gene is potentially targetable with small molecule drugs.
In fact, another drug that blocks the function of this molecular pathway, in addition to others, has already been tested in patients with myelodysplastic syndrome to induce cancer cell death.
“This gives us some confidence that more specific inhibitors can be discovered with improved safety profiles to be tested in settings where immunotherapy is sub-optimal and additional ways to enhance the immune response to cancer are needed,” Professor Huntington said.
In patients with colorectal cancers, the tumour cells produce higher amounts of IL-15 than other healthy tissues in their body.
Cancer cells can often mutate the IL-15 gene to blunt the immune response and this is linked to tumour recurrence and a poor prognosis in these patients.
Making immune cells exquisitely sensitive to the body’s own IL-15 has the potential to drive strong immune activation at sites of IL-15 such as colorectal cancer, while sparing other healthy organs where IL-15 levels are negligible.
Importantly, this newly identified way to harness the normal IL-15 pathway could be used in combination with existing gold-standard cancer immune checkpoint inhibitors, according to Jai Rautela, CEO of oNKo-Innate.
“Drugs that augment IL-15 signalling could add yet another layer of support to the anti-cancer immune activity in advanced tumours,” he said.
“This study is an important demonstration that deep immunology can generate new solutions to historically difficult biology, such as IL-15, and pave the way for next-generation immunotherapies.”


Max: 1500 characters
There are no comments yet. Be the first to comment.